Figures from ONS showed suicide rates have either increase or remained unchanged across the UK compared to 2022, with this in mind, Hertfordshire Partnership University NHS Foundation Trust (HPFT) has taken a critical step with the introduction of the Hertfordshire Suicide Prevention Pathway (HSPP) (1). From January 2024, HPFT began implementing the HSPP, locally adapted from the evidence based Australian Gold Coast Health & Hospital Service Suicide Prevention Pathway (GCSPP). Health Innovation East was commissioned to conduct a real-world evaluation (RWE) on the implementation of the HSPP. The evaluation sheds light on the early-phase implementation of this programme, revealing both progress and key areas for development. At its core, the evaluation tells a story of adaptive learning, staff engagement, and the essential conditions for sustainable system-wide change.
The adapted HSPP was co-produced by the Hertfordshire Mental Health, Learning Disability and Neurodiversity Health Care Partnership (MHLDA HCP), bringing together a diverse group of voices from across the system. From its earliest stages, this was a collaborative process that involved those with lived experience of suicide*, frontline staff, local leaders, and system partners.
* People with lived experience of suicide are those who have experienced suicidal thoughts, survived a suicide attempt, supported a loved one through a suicidal crisis, or been bereaved by suicide.
Building a Safer System: How Hertfordshire’s Suicide Prevention Pathway is Changing Mental Health Care
Within mental health service, suicide prevention is not just a clinical imperative – it’s a systemic challenge that requires coordinated effort, clear communication, and adaptive strategies. As part of a broader commitment to improving care pathways and reducing suicide risk, the HSPP was introduced within a complex, multi-agency mental health system.
The HSPP was developed in response to rising suicide rates nationally and locally (2). Furthermore, Hertfordshire Public Health Data showed increased deaths by suicide and gaps in follow-up care for those in crisis. Research revealed key issues in suicide prevention: poor risk detection, lack of targeted interventions, and insufficient care intensity (3). A 2025 service evaluation supported the pathway’s approach, emphasizing early identification, standardised screening tools, structured follow-up, and improved clinician awareness (4).
The HSPP is about creating structure in times of crisis. It’s designed to improve joined up care and ensure that individuals at risk of suicide do not fall through the gaps between services.
Health Innovation East's involvement
Developmental Evaluation in Action
Between April 2024 and February 2025, the HSPP was supported by a Developmental Evaluation approach —an approach suited to understanding complex programmes, a flexible evaluation and providing rapid feedback as findings emerge.
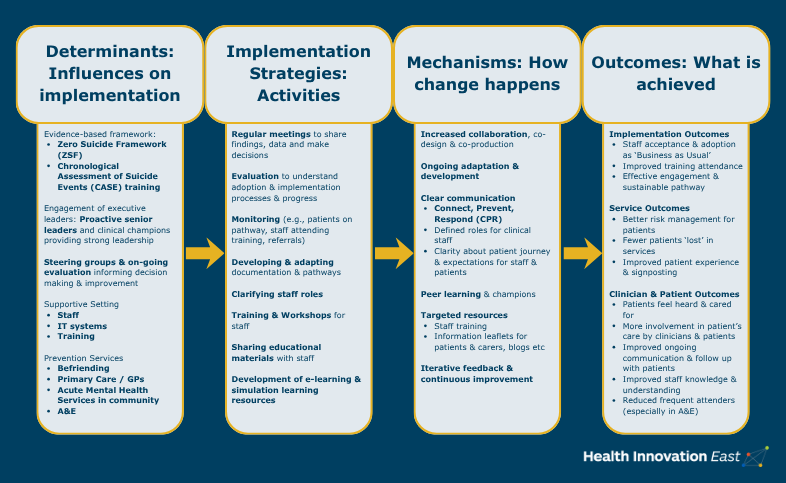
To unpack what drives or inhibits change, the RWE team applied two established frameworks, the Implementation Research Logic Model (IRLM) and the Theoretical Domains Framework (TDF) (5, 6). Through the lens of these frameworks, the RWE team identified key determinants and mechanisms that influenced implementation outcomes.
By engaging a wide range of staff through interviews and workshops, the team gathered rich, nuanced insights. Informal conversations proved particularly valuable in shaping both data collection and analysis, revealing practical concerns and real-world barriers that might have otherwise gone unnoticed.
Continuous feedback loops between the RWE team and the implementation team ensured that emerging themes informed live decisions, making the evaluation a vital part of the implementation journey. As a result, implementation was an iterative process, characterised by growing staff engagement, rising patient numbers entering the pathway, and ongoing adjustments in implementation strategy.
Since implementation of the pathway, an increasing number of patients have been appropriately placed on the suicide prevention pathway, leading to more timely interventions and improved continuity of care.
Feedback from the evaluation helped inform the leadership team to refine training materials, communication strategies, and engagement methods as challenges emerged.
Staff engagement increased, with growing participation in targeted training. Simulation-based learning in particular was well received, helping staff build confidence in responding to complex scenarios, including in a high-pressure mental health environment.
The HSPP has been implemented across:
- A&E Watford General
- A&E, Lister Hospital
- Mental Health Urgent Care Centre, Lister Hospital
- Mental Health Liaison team at Lister Hospital
- All Crisis Resolution and Home Treatment (CRHT) teams in HPFT
- Referral pathway to the Mind Befriending service, funded by Hertfordshire County Council Public Health
Other health systems in England and internationally have expressed interest to the team in Hertfordshire to learn more to support their adoption of a similar pathway.
Health Innovation East are continuing to work with the HSPP team to produce resources to support wider adoption, including a summary sheet of findings to act as a guide to early implementation. View the visual summary and logic model here.
HSPP have now launched a new evidence-based e-learning module on the suicide prevention pathway. Co-produced with experts by experience and system partners, ensuring it is grounded in real-world insights and best practices, it is built on the Connect, Prevent, Respond approach. This valuable resource is accessible to all staff and communities via the NHS Learning Hub or staff ESR account.
Foundations for Sustainable Change
One of the evaluation’s strongest messages is that sustainable change requires action across multiple levels: individuals, teams, organisations, and the wider system. Staff behaviour, peer learning, workflow redesign, inter-team communication, and system alignment all play a role.
To build on early successes, the evaluation lays out clear and actionable recommendations:
- Enhance understanding across staff and systems
- Tailor training to meet staff needs
- Integrate the pathway into existing structures
- Foster multi-agency collaboration
- Encourage peer learning
Looking Ahead: A Blueprint for Others
The HSPP and findings from the evaluation offers guidance for other trusts and similar health systems looking to implement suicide prevention pathways. Recommendations reflect an approach to implementation that values co-production, recognises contextual nuance, and the centrality of leadership and engagement to sustained change.
Tailoring interventions to the specific team context, clarifying roles early, peer learning, and highlighting tangible benefits for staff and patients are all identified as best practices for future adopters.
References
References
(2) https://pubmed.ncbi.nlm.nih.gov/38742289/
(3) Center for Mental Health Services (US): Office of the Surgeon General. National Strategy for Suicide Prevention: Goals and Objectives for Action. Rockville (MD) US: US Public Health Service; 2001.
(4) Anstee L, Richards S, Shah C, Magon R, Zia A. Characteristics and outcomes of people in suicidal crisis at two emergency departments: a service evaluation. Emergency nurse. 2025;33(1).
(5) Smith JD, Li DH, Rafferty MR. The implementation research logic model: a method for planning, executing, reporting, and synthesizing implementation projects. Implementation Science. 2020;15:1-12.
(6) Atkins L, Francis J, Islam R, O’Connor D, Patey A, Ivers N, et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implementation science. 2017;12:1-18
Share your idea
Do you have a great idea that could deliver meaningful change in the real world?
Get involved