Health Innovation East’s 2024 Autumn Innovation Showcase connects innovators, accelerates learning and delivers rich conversations.
Our Autumn Innovation Showcase, held on 14 November, 2024 at the Babraham Research Campus, connected senior executives from across health and social care at a regional and national level with companies and colleagues who have already started to land their innovations in the health and care system. As well as looking ahead to their next steps to scale, the innovators and health systems represented shared valuable insights for others working to ensure that great ideas make a difference for the people places and problems where they are needed most.
To find out more about Health Innovation East’s work with health and care innovators please contact enquiries@healthinnovationeast.co.uk
Interesting threads from the day included:
Innovate at pace, but never in isolation – it is imperative that innovators work with health system colleagues to understand how their innovation fits within broader care pathways and the shifting regulatory landscape.
The NHS will need to adapt and evolve to leverage the potential of Artificial Intelligence (AI). However, we must work with our systems and the people that make them work at all levels – infrastructure, training and transparent dialogue with staff and patients will help drive transformative solutions.
Nationally there is a thirst for strategy and frameworks that allow the system to be agile in its response to new technologies. A refreshed 10-year plan may offer innovators the assurance that they are aligned with the long term direction of the health and care system, but it should not impose limits on creativity through being excessively prescriptive.
Shifting the narrative and the funding towards successful implementation.
Piers Ricketts, Chief Executive, Health Innovation East.
Much has been written about the state of the NHS following the arrival of the new government, the publication of Lord Darzi’s review of the NHS, the Innovation Ecosystem Programme (IEP) report and the forthcoming 10-year plan.
It is highly likely that the 10-year plan will draw on some of the IEP’s conclusions: indeed, a separate paper on the implementation of innovation is being prepared alongside the plan. The recent budget granted the NHS an additional £22 billion of funding, but the NHS is likely to be required to demonstrate the improved outcomes that it will achieve with this increase, notwithstanding the fact that much of the increase will be used to cover recent pay settlements. In this context, new health technologies and care pathways will have to demonstrate their benefits to patients and the NHS more strongly than ever. By the same token, the required improvements in outcomes will only be achieved with more widespread use of technologies that have been proven to work but have not yet been sufficiently deployed at scale.
At the centre of the event, seven early-stage health technology companies presented on their experience in successfully implementing their innovations into the NHS. Each was founded to solve a ubiquitous issue, and all have taken a highly practical approach to implementation. Thought-provoking keynote speakers from NICE, NHS England and the Tony Blair Institute also shared their thoughts on the policy and regulatory changes they believe are needed to help the NHS to deliver on its mandate in the coming years.
Reflections from our keynote speakers – helping the NHS deliver its mandate
Early Value Assessments promise to accelerate the most needed innovations, without compromising standards
Jo McCormack, Implementation Consultant, National Institute for Health and Care Excellence (NICE).
NICE helps practitioners and commissioners to get the best care to people fast. It provides clear guidance on high priority health topics driven by the robust evidence it collects along with its partners. NICE acts to encourage the uptake of best practices to improve outcomes for all.
Outlining the wide range of guidance and services NICE provides, Jo described how it is working to make it easier for commissioners, practitioners and patients to access and decide on treatment options. The audience was clearly pleased to see NICE represented, particularly when Jo elaborated on the role of Early Value Assessments (EVAs), MultiTech Guidance (MTG) and Late-Stage Assessments (LSAs) which combine to develop an increasingly integrated MedTech pathway. Jo walked the audience through how NICE has listened closely to health and care systems in the development of EVA’s, which accelerate the progress of promising innovations working in areas of greatest need.
In concluding, Jo set the audience a challenge – to provide case studies from the East of England that share learning around the implementation of innovations and their impact on patient journeys and outcomes.
Personal reflections on innovation
Christina Farrow, Deputy Director of Innovation, NHS England
Christina shared an analogy that immediately engaged the audience, drawing parallels between her recent experience of building a house and the journey of implementing innovation into the NHS. She reminded us that building a home or an innovation is rarely easy or glamorous. Emphasizing the importance of ‘finding your people’, Christina spoke to the need to surround oneself with the right people, knowledge and expertise to make progress – particularly important for building the resilience to interrogate problems and find solutions when things go wrong.
With these factors in place, supported by a long-term vision and the agility to meet the requirements of shifting regulatory landscapes, attendees were encouraged to connect with Christina’s steadfast belief that embedding innovation within our healthcare system and driving change for patients is entirely achievable. Much like building your own Grand Design!
Artificial Intelligence is already driving prevention and productivity in healthcare system around the world, what about the NHS?
Charlotte Refsum, Head of Health Policy, Tony Blair Institute for Global Change
In a thought-provoking presentation and conversation, Charlotte covered wide-ranging topics from the importance of innovations in healthcare systems as drivers of economic growth and prosperity, to the ways in which global health systems are preparing for the AI era.
Our Q&A conversations captured the importance of implementing AI with local health care systems as active partners rather than subjects. Charlotte’s presentation had a more international scope, she articulated the opportunity for AI to address future global demand and capacity challenges – from helping prevent incidences of communicable disease (including pandemics and antimicrobial resistance), to supporting productivity and efficiencies in workforces and less efficient models of care. Examples from around the world included operational gains in Canada, policy development in Finland, public health messaging in South Korea and the development of precision medicines in China. Charlotte concluded with an eight-item framework to ‘stimulate, regulate and assimilate’ AI, including, but not limited to:
- Data and digital infrastructure – including 5G network capability.
- Data sharing and interoperability – encompassing Open Standards.
- Innovation support – highlighting the importance of AI strategy.
- Regulatory frameworks – comprising ethics, bias, privacy, security and trust.
- Adoption and spread – emphasising the role of innovation agencies such as the Health Innovation Network.
- Workforce agility – planning upskilling and pathway design.
- Primary care infrastructure – integrating omni-channel access and Polyclinics.
- A risk pooling function – seeing the state ensure the vulnerable are not left behind.
Innovator’s implementation insights:
Stasis in the care pathway creates an opening for innovation
Caroline Cake, Co-Founder and CEO, Neu Health
After witnessing both her grandmother and mother face the challenges of dementia, Caroline was struck by the lack of progress in its management over the years. The Parkinson’s care pathway is structured around specialist appointments every six months to a year to assess symptoms and appropriate treatment: Neu Health is a smartphone-based app to track Parkinson’s Symptoms designed to work within the pathway. The app not only empowers patients and carers, but also uses AI and Machine Learning to provide clinician insights to a patient’s condition to help inform symptom management and appointment frequency. Just a few days after Neu health presentation they attended and won the 2024 HSJ Award for Digitising Patient Care. Find out more about how Neu Health is transforming care and outcomes in the East of England.
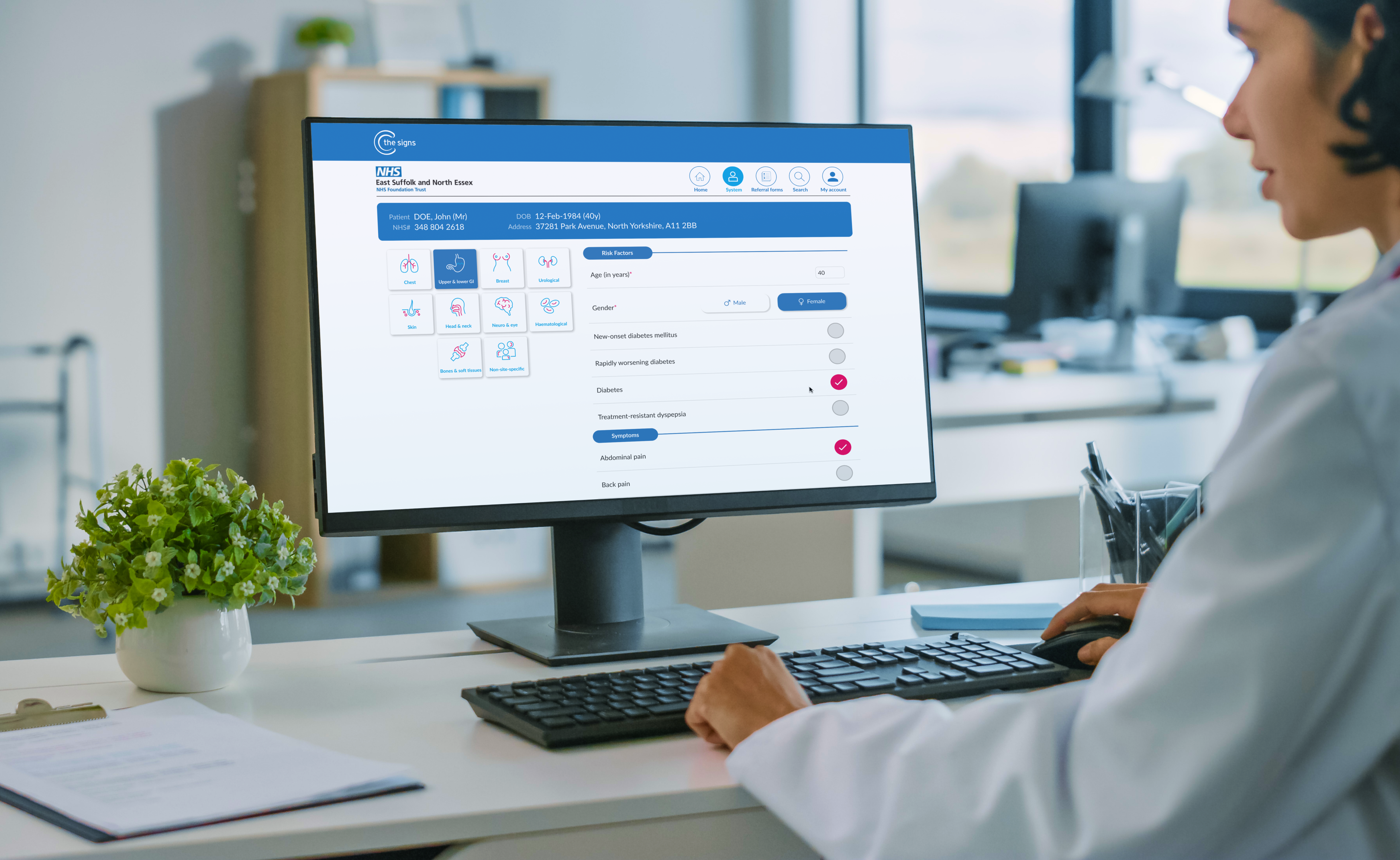
A practical solution: using AI to improve early cancer diagnosis
Bea Bakshi, Co-Founder and CEO, C the Signs
Bea established C the Signs, when she was a GP, in response to delivering a cancer diagnosis to a patient who asked, “why wasn’t this picked up sooner?” With only 25% of cancers currently eligible for screening and 56% of cancers missed in primary care, the urgency for innovation is clear. C the Signs is a cancer prediction service which supports GPs by rapidly identifying which cancers a patient is at risk of and recommending the most appropriate test or specialist. With a 99% sensitivity score (meaning it detects 99% of all cancers), C the Signs offers a practical solution to support the NHS Long Term plan’s commitment to achieving 75% of cases diagnoses at stage 1 or 2 by 2028. Read more about an independent evaluation that shows the potential for C the Signs to improve cancer detection rates by 12%.
Placing point of care within community settings increases engagement for improved health outcomes
Luke Dawson, Partnerships Manager, PocDoc
Rethinking how services are delivered can transform access to care for those often labelled “hard to reach.” By meeting people where they are, we can connect with individuals who may never or rarely engage with traditional healthcare settings. PocDoc exemplifies this approach, conducting cholesterol assessments through a 7-minute point-of-care test across the North East and North Cumbria. Results show that 30% of participants at outreach events – held in environments such as football matches and farmers markets – had never been assessed before. This model demonstrates how by bringing the right tools into communities we can significantly expand access and improve public health outcomes. Health Innovation East is supporting PocDoc’s work in the East of England.
Leveraging pilots provides implementation insights to fast track adoption
Gabriel Lambert, Director of Clinical and Commercial Development, TidalSense
TidalSense is working to respond to patients who present symptoms of Chronic obstructive pulmonary disease (COPD) but have not been diagnosed, by improving spirometry for patients and clinicians. N-Tidal Diagnose, a point of care diagnostic solution, improves patient experience, takes 10 minutes and can be administered by health professionals at many levels to help address the waitlist exacerbated by COVID-19. Gabriel emphasised the power of piloting innovations to address specific questions: TidalSense have leveraged their pilots to find solutions to potential constraints in test administration and providing the training necessary to empower staff to work with AI powered results. Working proactively to understand barriers to implementation and gain usability data can help fast track adoption later down the line.
A network approach brings the expertise necessary to accelerate rare disease diagnosis time
Peter Fish, CEO, Mendelian
When viewed collectively, rare diseases have a larger impact than the name suggests, affecting one in 17 people at some point in their life and with an average diagnosis time of five years. MendelScan is a clinical decision support system which runs case-finding algorithms on anonymised electronic health records to identify potential patients and enable faster diagnosis. If identifying individual rare disease cases can be compared to looking for needles in a haystack, Peter articulated that part of the challenge is actually “getting the haystack to look for needles”: leveraging partners such as Secure Data Environments is essential to improve health outcomes across the population. With cases identified, part of Mendelian’s implementation journey has been to develop operational delivery networks to ensure access to specialist support and expertise regardless of a patient’s location.
Improving access to primary care
Kristiaan Van Driem, UK Sales and Marketing Director, Klinik Healthcare Solutions
Access to primary care is a concern that resonates with many. However, there are significant gaps in availability, convenience, and patient satisfaction. By asking the right questions at the point of access and automating processes, it is possible to enhance patient flow and improve the efficiency of many patient-led primary care engagements or self-referral services.
Klinik delivers an AI-powered online triage and patient flow management solution for NHS GP practices & PCNs. By capturing the right quality of information at first contact, Klinik reduces GP visits and optimises demand management, showing how AI can enhance patient experience and staff efficiency. Working with Portland Medical Centre, the Klinik system saved between three and four GP sessions per week, despite increased demand.
More than just a “no show”: using AI to predict environmental barriers for improved patient outcomes and system resourcing
Benyamin Deldar, Co-Founder and Co-CEO, Deep Medical
Missed appointments represent a significant risk marker for all-cause mortality, and patients from minority and marginalised communities are disproportionately affected in this way. Without accessing patient-identifiable or medical information, Deep Medical has demonstrated the power of using predictive analytics to enhance healthcare utilisation. By leveraging data on behaviours and the environment such as traffic conditions and the weather, Deep Medical can work with health and care providers to forecast healthcare needs and optimise resource allocation.
Simultaneously employing dynamic scheduling and personalised messaging can reach underserved populations and improve their clinical outcomes, for example Deep Medical connects Webex and Uber to get transport to patients that need it. In Mid and South Essex, Deep Medical have increased attendance at appointments by 30% for patients from the 20% most disadvantaged communities.
To discover more about Health Innovation East’s work in the East of England read our 2023/24 Impact review here. At Health Innovation East we are clinicians, data scientists, industry experts and programme leaders. We are passionate about getting the best innovations in health and care to the people places and problems where they are needed most. Our consulting services encompass innovation, health informatics, real-world evaluation and heath and care. We offer the capacity and knowhow to transform how health and care is delivered.
Note: the points above were taken from the presentations: whilst Health Innovation East or other member organisations in the Health Innovation Network have worked closely with the presenting companies, Health Innovation East has not sought to verify the specific assertions below with reference to the respective company websites and underlying source material where relevant, except where indicated.
You might also like…

Amy Miller, senior advisor at Health Innovation East shares considerations for the implementing of digital healthcare technologies in order to avoid widening healthcare inequalities for children and young people.
Share your idea
Do you have a great idea that could deliver meaningful change in the real world?
Get involved