The equitable distribution of funding and knowing what actually works are important to help primary care practitioners address the challenges posed by health inequalities.
In primary care, the way that funding is distributed for general practice funding is well established nationally – with the variant of the Carr-Hill formula (1), but for discretionary additional funds there is no national guidance on how best to distribute them. Seemingly, the easiest solution is for the allocation of funding to be based on per head population. However, as part of the NHS Long Term Plan, addressing and tackling health inequalities is a key priority for this decade. Therefore, it is vitally important that when allocating funding underlying inequalities are considered, which makes the equitable distribution of funding all the more difficult.
In the current financial climate we are all very aware of how budgets are being tightened and that discretionary funding does not come around very often, which makes it all the more important that when funding is available it can have the biggest possible impact for the people, place and problems where it is needed most. In addition, there are often requirements for spending the money within very short timelines. Recently, Integrated Care Boards (ICBs) and Health Innovation Networks across the country have been working on NHS England’s Innovation for Healthcare Inequalities Programme (InHIP), which provided £100,000 to ICBs (a total of £4.2 million nationally) to support the access of selected innovations to targeted cohorts from CORE20Plus5. On receiving InHiP funding ICBs had to rapidly identify not only which groups they hoped to improve access to, but also the geographical locations that they wished to approach. Whilst guidance was made available for the technologies and cohorts, ICBs were given the autonomy to determine the geographies where the programme could have the most impact.
Equity vs. Equality: Understanding the Difference
When considering the provision of funding, it’s important that we make the distinction between equity and equality. While equality implies providing the same level of resources to all GP surgeries, equity involves tailoring the distribution of resources to address specific needs and circumstances. For instance, a GP surgery in a socioeconomically deprived area may face greater challenges and higher demand for services than one in a less deprived neighborhood. An equal distribution of funding would be less likely to consider such differences, potentially exacerbating existing inequalities. In contrast, an equitable approach would allocate more resources to the surgery in the deprived area to address its higher level of need.
However, to take into consideration the various indices that impact inequalities, complex formulas need to be used, and if those looking to consider inequalities in their work would like to weight the indicators then the complexity increases further. Whilst working with Cambridgeshire and Peterborough Integrated Care Board, John Ford, Senior Clinical Lecturer in Health Equity at Queen Mary University London, and colleagues, developed a formula (image 1 below) that could take into account several indicators of health inequality, GP practice lists, indices of deprivation (and how much impact they should have on the formular) and funding available to provide guidance on how to distribute funding via an equitable lens.
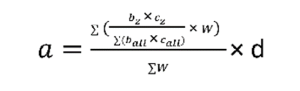
However, pulling together all of the indicators, determining weightings and double checking that the formula is inputted correctly takes time – and like all things leaves open the potential for human error. In order to support ICBs in using this formula, and help save them time and resources when allocating funding, Peter Saiu, Deputy Head of Business Intelligence NHS England, has developed the eFIT tool. Saiu’s online tool brings together a variety of different inequality indicators and ICB data into an easy to use app that creates a simple and accessible guidelines for ICBs on how funding could be distributed equitably. In addition, the tool has the ability to upload and incorporate of local indicator data, allowing for further customisation, and accuracy.
The formula behind the tool has already been used successfully at C&P ICS in improving uptake and coverage of Faecal Immunochemisty tests (FIT), which are at-home testing kits sent to eligible members of the public that detect markers early for bowel cancer. The project resulted in improved uptake across all GP practices in Cambridgeshire and Peterborough, clearly demonstrating that by allocating funding in a more equitable way all practices were able to improve instead of only those in the more affluent areas as is frequently seen (2)
It’s vitally important to remember that the equitable distribution of funding is only part of the battle. Without any practical ways of reducing health inequalities, the funding will not be able to have as large an impact as it could. To help support reducing inequalities in primary care the Health Equity Evidence Centre (HEEC) has been created.
While working to address inequalities, John Ford identified that whilst there was a wealth of evidence describing the problems, there was comparatively little work being done on collating and understanding “what works” in primary care. To address this, John and his team of researchers, practitioners and computer scientists, supported by innovative AI-based methodologies, have created a living evidence map of what works in primary care settings – allowing ICBs to review the available evidence across a variety of different demographics, interventions, and areas of practice. To further support the ICBs, and to reduce workload and duplication of effort, the team also create “Evidence Briefs”. The briefs pull together all the available evidence on specific areas (e.g. Cholesterol management) and identify which interventions work best in primary care.
Dr Gary Howsam, chief clinical improvement officer at Cambridge and Peterborough ICS and non-executive director at Health Innovation East says of the HEEC
“Having an evidence-based, collective understanding of where to focus efforts for maximum impact is invaluable. Utilising this knowledge to enable primary care teams to concentrate their efforts on the areas which the evidence shows will lead to ‘wins’ for their population will help maintain engagement and momentum and widen participation in this important work”.
Together, these two initiatives are helping make the provision of primary care services increasingly equitable across Cambridgeshire and Peterborough. Supported by us Health Innovation East and other key regional partners the teams work will have a positive impact on health inequalities every day.
References
1- British Medical Association. (2024). Global sum allocation formula. [Online]. www.bma.org.uk. Last Updated: 19 August 2024. Available at: https://www.bma.org.uk/advice-and-support/gp-practices/funding-and-contracts/global-sum-allocation-f [Accessed 15 September 2024].
2- Barr B, Bambra C, Whitehead M. The impact of NHS resource allocation policy on health inequalities in England 2001-11: longitudinal ecological study. BMJ. 2014 May 27;348:g3231. doi: 10.1136/bmj.g3231. PMID: 24865459; PMCID: PMC4035504.
You might also like…
Share your idea
Do you have a great idea that could deliver meaningful change in the real world?
Get involved

