Adhering to medication regimes is crucial for children and young people (CYP) with epilepsy to both maximise their overall health and wellbeing and fulfil their potential. However, evidence tells us that adherence can be poor (Paschal et al, 2016).
The NHS England East of England CYP Programme commissioned Health Innovation East to identify enablers and barriers relating to medication adherence and find solutions to support better adherence.
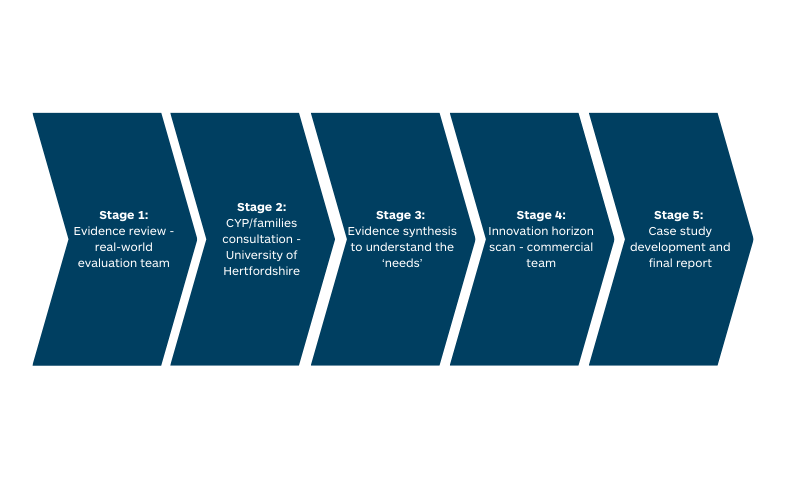
The project encompassed a rapid review of the academic literature, qualitative research exploring the views of CYP with an epilepsy diagnosis and their parents and carers and a horizon scan identifying technologies to improve adherence.
Using evidence to analyse and address gaps in existing healthcare provision is an example of how Health Innovation East is positioned to respond to the demands within health and care systems.
Insight
Epilepsy is a long-term condition that affects approximately 112,000 children and young people in the United Kingdom (1). It is identified as one of the five conditions in NHS England’s CYP Core20PLUS5 document (2). CYP who live in areas of deprivation are more likely to receive a diagnosis of epilepsy and those who have the condition are more likely to have neuro-developmental conditions (3).
Engaging colleagues at the University of Hertfordshire, Health Innovation East conducted a scoping review of the evidence to identify influences on medication adherence and any best practice approaches. After screening 2,639 studies, 20 were considered eligible studies for the review.
Following the evidence review we were able to:
- Describe the factors which influence medication adherence for young people with paediatric epilepsy.
- Describe any factors influencing variation in how young people adhere to epilepsy medication.
- Report on best practice in supporting patients, parents and carers with young people’s adherence to epilepsy medication.
On behalf of Health Innovation East, our University of Hertfordshire partners used the review findings to design the interview question schedule used for 22 semi-structured interviews with children and young people and their caregivers.
The aims of the CYP interviews were to gain insight and understanding of:
- The facilitators and barriers to epilepsy medication adherence in CYP.
- How those barrier(s)could be addressed.
- The changes required to facilitate good epilepsy medication adherence – taking medication as prescribed.
Our partnership resulted in a report ‘Medical adherence in paediatric epilepsy’ (MAPE) published on the NIHR ARC East of England website.
Experiencing epilepsy
“Yes, so I’m in Year 11 and it can be quite stressful like thinking what if I’m in an exam and the medication doesn’t work or something and I have a seizure. And then like if I have a seizure when I’m at home which happened I think like two weeks ago, I couldn’t go into school the next day, so I missed a lot of work and that was quite stressful as well.” Young person
“Yeah I did forget to take the medication. It was sometimes quite frequently but then it didn’t happen so often like after that, because obviously my dad had to continue to remind me and it was the same as the tablets I was on, like my iron. Because I’d just wake up, I was tired, I was in a rush to get to school, I had to get ready, I was already out the door, so my brain didn’t have really that much time to like think about what…I need to get this done, because I didn’t have time. So I’d just forget it out rush.” Young person
“It [the diagnosis] was just so overwhelming…I don’t mind telling people, I had to go on anxiety medication, it’s really affected my mental health…I actually had time out of the NHS because I couldn’t go to work.” Parent / Carer
Intervention
The project encompassed a rapid review of the published literature, qualitative research seeking the views of CYP with an epilepsy diagnosis and their parents or caregivers and a horizon scan to identify technologies which could potentially improve adherence.
Following approval of the two reviews, an evidence synthesis (the process of gathering, analysing, and integrating findings from multiple studies on a particular topic) was completed to consolidate the findings into a set of ‘needs’. The needs were further refined via a collaborative workshop into need statements, in order to focus the efforts of an innovation horizon scan.
’A way to help CYP and their families to remember all medication doses in order to support medication adherence’
’A way to address unmet information needs for CYP and their families in order to provide tailored and responsive advice to support medication adherence’
The detailed final summary report is due during Summer 2025.
We have been collaborating with Health Innovation East on a study focusing on medication adherence in children and young people who have epilepsy. Health Innovation East have been highly professional and organised; at the same time, they have adopted a supportive listening approach that is receptive to suggestions and ideas. It is an absolute pleasure to work with them.
Associate Dean of Research, School of Health and Social Work, University of Hertfordshire
Impact
The comprehensive scoping review identified factors influencing how and when people take medication and suggested best practice approaches for improving medication adherence in young people.
For young patients: Improve patient knowledge and empowerment about the condition, importance of adherence and ways they can help to self-manage.
For families: Increase early and ongoing family centred care and support from healthcare professionals (HCP)s, improve parent /caregiver knowledge and empowerment, encourage parents/carers to develop schedules or prompts reminding patients to take medication.
For clinicians: Improve knowledge and early identification of factors influencing adherence, respond to individual needs and provide tailored patient care, assess and review children’s needs throughout the disease course, provide telephone reminders for appointments, provide less complex treatment regimens where possible and offer psychosocial input for young people.
For health and care systems: Improve accessibility/equity of medications for patients and their carers, explore further integration between hospital and community services around epilepsy.
The 21 semi structured interviews with children and young people and caregivers provided an invaluable insight into managing epilepsy medication adherence. The key findings revealed:
Children and young people
- The children and young people’s knowledge of their epilepsy medication and how it works was limited and their medication adherence could be impacted by a change in their daily routine. All participants reported that parental support played a substantive role in medication administration and ensuring that the prescribed regime was adhered to.
Parents and carers
- Parents had a thirst for information that related to their child’s epilepsy and their medication regime; however, they were not always aware of how to access appropriate resources, meaning that they frequently turned to charity websites and relevant Facebook pages.
- Parental knowledge of their child’s epilepsy drugs, and how they worked, was limited.
- Involvement in healthcare decision-making processes was important for the participants, particularly building a trusting and therapeutic relationship with practitioners, such as the medical consultant and epilepsy nurses.
- Parents reported that the diagnosis and management of paediatric epilepsy impacted their family’s lives, in terms of parental emotions and the forward planning required to maintain parental vigilance and medication adherence.
Using this evidence and addressing the recommendations from these reports has the potential to improve medication adherence.
Creating accessible and targeted information resources for CYP and their families – such as personalised guidance from healthcare professionals, interactive education platforms, or community-led initiatives – would meet their unmet informational needs.
Implementing innovations and systems, such as reminders or alarms tailored to individual routines, may help ensure medication doses are remembered and taken consistently, mitigating disruptions caused by changes in daily schedules. These types of interventions have the potential to improve medication management and quality of life for affected families. However, it is clear that a combination of tools and strategies may be required.
Next steps
Following full consultation via the MAPE steering group on the innovations identified, Health Innovation East is developing a set of case studies, incorporating real-world examples, of successful approaches to improving children and young people’s medication adherence. With the completion of the case studies will come a final MAPE report, bringing together all the project recommendations, which will be shared with the NHS England CYP’s team. Further and finally, Health Innovation East will plan and deliver a comprehensive knowledge mobilisation plan ensure the findings are shared with other regions across England in a way that is accessible, relevant and tailored to all key stakeholder groups.
Read the summary report
Find out more by reading the Medication Adherence in Paediatric Epilepsy: summary report
References:
References:
(1) NHS England. (2023). National bundle of care for children and young people with epilepsy. [Online]. england.nhs.co.uk. Last Updated: 30 November, 2023. Available at: https://www.england.nhs.uk/long-read/national-bundle-of-care-for-children-and-young-people-with-epil [Accessed 11 April 2025].
(2) NHS England. (2022). Core20PLUS5 infographic – Children and young people. [Online]. england.nhs.uk. Last Updated: 18 November 2022. Available at: https://www.england.nhs.uk/publication/core20plus5-infographic-children-and-young-people/ [Accessed 9 April 2025].
(3) Paschal, A.M et al. (2016). Parent health literacy and adherence-related outcomes in children with epilepsy. Epilepsy & Behavior. 56(March 2016), pp.73-82. [Online]. Available at: https://www.sciencedirect.com/science/article/abs/pii/S1525505015006915 [Accessed 11 April 2025].